Living with Polycystic Ovary Syndrome (PCOS) can feel like a lifelong journey. Understanding the nuances of this condition is crucial for effective management and leading a fulfilling life. This article delves into the intricacies of PCOD, shedding light on its lifelong nature, impacts, management techniques, and more.
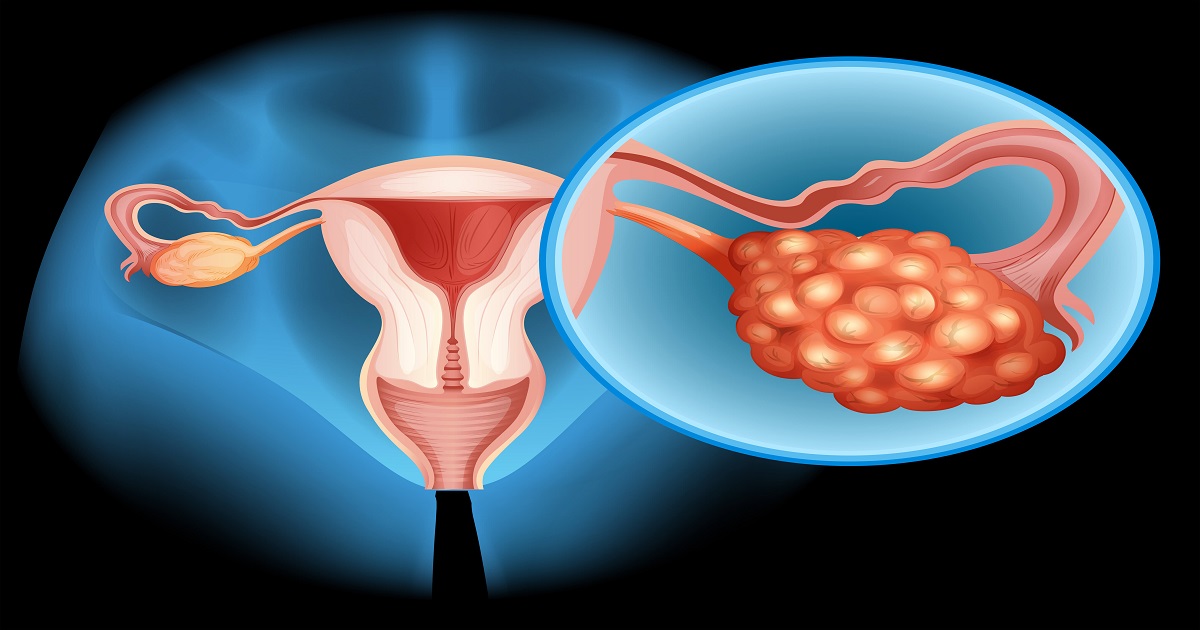
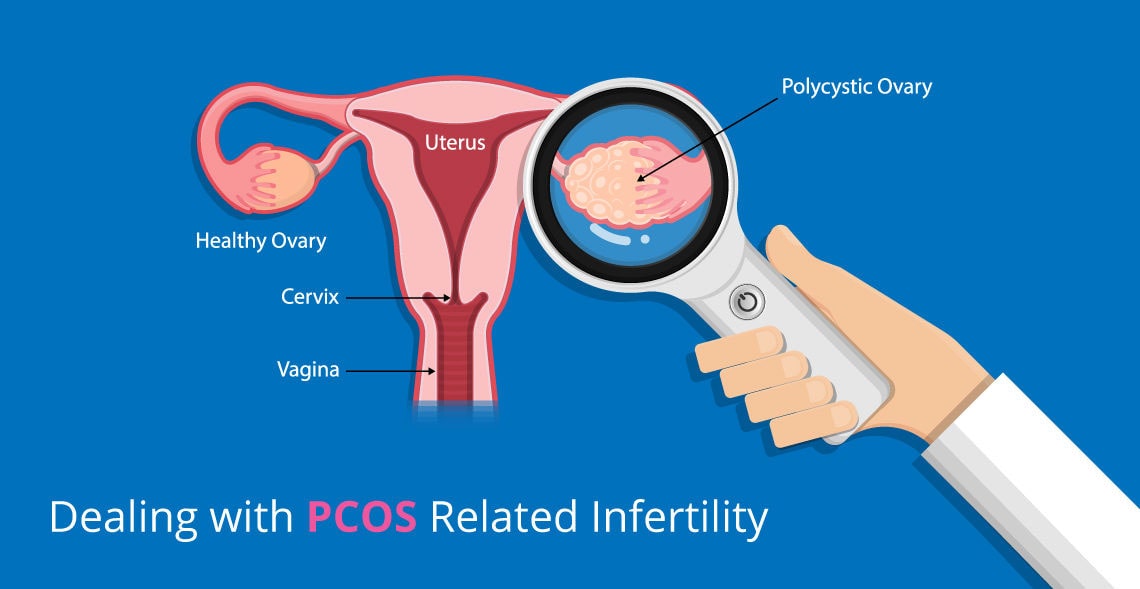
Polycystic Ovary Syndrome (PCOS) is a lifrstyle disorder which occurs due to imbalance of the harmones. It is characterized by irregular menstruation, excess androgen levels, and polycystic ovaries.PCOS is a multifaceted condition with various symptoms, including irregular periods, excessive hair growth, acne, and weight gain. Understanding these symptoms is crucial for early diagnosis and effective management.
PCOD isn't just a phase; it's a lifelong companion for many women. While symptoms may fluctuate over time, the underlying hormonal imbalances persist, necessitating long-term management strategies.The hormonal imbalances in PCOD, such as insulin resistance and androgen excess, contribute to its chronic nature. Therefore, adopting a proactive approach to managing PCOD is essential for long-term well-being.
The ramifications of PCOD extend beyond physical health, affecting various aspects of daily life. From managing symptoms like fatigue and mood swings to coping with fertility concerns, PCOD can significantly impact emotional and mental well-being.Navigating these challenges requires resilience and support from healthcare providers, family, and peers. By fostering open communication and seeking appropriate resources, individuals with PCOD can enhance their quality of life.
Diagnosing PCOD involves a comprehensive evaluation of symptoms, medical history, and laboratory tests. Since symptoms vary widely among individuals, healthcare providers employ a tailored approach to diagnosis.Blood tests to assess hormone levels, pelvic ultrasound to examine the ovaries, and exclusion of other conditions with similar symptoms are integral parts of the diagnostic process.
PCOD management is not one-size-fits-all; it evolves with age and life stages. From adolescence to menopause, individuals with PCOD require personalized strategies to address changing hormonal dynamics and health needs.Early intervention with lifestyle modifications, such as regular exercise and balanced nutrition, can mitigate symptoms and prevent complications in the long run
Optimal nutrition plays a pivotal role in managing PCOD symptoms and promoting overall well-being. Emphasizing whole foods, fiber-rich fruits and vegetables, and lean proteins can help regulate insulin levels and promote weight management.Lifestyle modifications, including stress management techniques and adequate sleep, complement dietary changes, fostering a holistic approach to PCOD management.
In addition to lifestyle modifications, medications and treatments may be necessary to alleviate specific PCOD symptoms and prevent long-term complications.Birth control pills, anti-androgen medications, and insulin-sensitizing agents are commonly prescribed to correct menstrual cycles,decrease androgen levels, and control insulin sensitivity.
Living with a chronic condition like PCOD can take a toll on mental health. Coping with the physical symptoms, fertility concerns, and societal stigmas associated with PCOD requires resilience and support.Seeking counseling, joining support groups, and practicing self-care are vital for nurturing psychological well-being and fostering a positive outlook on life.
Fertility challenges are a significant concern for women with PCOD. Irregular ovulation, hormonal imbalances, and ovarian cysts can hinder conception and increase the risk of miscarriage. However, with timely interventions, such as ovulation induction medications and assisted reproductive technologies, many women with PCOD can fulfill their dreams of parenthood.
Advancements in PCOD research offer hope for improved diagnostics and treatment modalities in the future. From unraveling genetic predispositions to exploring novel therapeutic targets, ongoing research endeavors aim to enhance the management and outcomes of PCOD.By staying informed about emerging research findings and participating in clinical trials, individuals with PCOD can contribute to the collective knowledge base and potentially benefit from innovative interventions.
Navigating the complexities of PCOD requires a multifaceted approach encompassing physical, emotional, and psychological well-being. Adopting coping strategies tailored to individual needs and preferences can empower individuals to thrive despite the challenges posed by PCOD.From practicing mindfulness and engaging in regular physical activity to fostering meaningful connections and seeking professional support, exploring diverse coping mechanisms is essential for enhancing resilience and reclaiming agency over one's health and life.
Living with PCOD is undoubtedly a challenging journey, but it's also an opportunity for growth, resilience, and empowerment. By understanding the lifelong nature of PCOD, adopting proactive management strategies, and nurturing holistic well-being, individuals can navigate the complexities of this condition with confidence and grace.
Living with PCOD (Polycystic Ovarian Syndrome) can be challenging, but there are natural ways to alleviate its symptoms and improve your quality of life. In this comprehensive guide, we'll explore 10 effective methods backed by expert advice to help you manage PCOD naturally.
PCOD is a hormonal disorder that affects women of reproductive age, causing irregular periods, infertility, and other health issues. Despite its prevalence, many women are unaware of how to effectively manage PCOD without resorting to medication or invasive treatments.
PCOD is believed to be caused by a combination of genetic, hormonal, and lifestyle factors. Insulin resistance, excess androgen production, and inflammation are among the primary contributors to this condition.
PCOD can have a significant impact on a woman's physical and emotional well-being. From menstrual irregularities to fertility problems and weight gain, PCOD symptoms can affect various aspects of daily life.
Diagnosing PCOD typically involves a combination of medical history review, physical examination, and diagnostic tests such as blood tests, ultrasound, and hormone level assessments.
Now, let's explore 10 natural strategies to effectively manage PCOD symptoms and promote hormonal balance:

Dealing with heavy menstrual bleeding can be challenging, but knowing when it's time to worry is crucial for your health and well-being. In this comprehensive guide, we'll delve into the intricacies of heavy menstrual bleeding, offering insights, tips, and expert advice to help you navigate this common but concerning issue.
Heavy menstrual bleeding, also known as menorrhagia, is a common problem affecting many women. It's characterized by excessive blood loss during menstruation, leading to prolonged periods and often interfering with daily activities. While occasional heavy bleeding may not be a cause for concern, persistent and excessive bleeding could indicate an underlying health issue.
When it comes to heavy menstrual bleeding, it's essential to recognize the signs and symptoms that may indicate a problem. These can include:
Understanding these signs can help you identify when your menstrual bleeding may be cause for concern.
Several factors can contribute to heavy menstrual bleeding. These include:
Identifying the underlying cause of your heavy menstrual bleeding is crucial for effective treatment and management.
When to Worry About Heavy Menstrual Bleeding While occasional heavy periods are normal for many women, certain signs may indicate that your bleeding warrants medical attention:
Effective management of heavy menstrual bleeding often involves a combination of lifestyle changes, medication, and, in some cases, surgical intervention.